Cancer Survivor, Weight Gain, Debilitating Back Pain, Swelling in Legs
Presentation – 72 y.o. female; prior patient (quit care in 2017 for unknown reasons). Since then, she had a stent, ovarian cancer, breast cancer and kidney cancer. All have been treated and “in remission”. On a combination of 10 medications (OTC and prescribed), plus Caltrate, Centrum Silver and Vitamin D.
Suffering from back pain, knee pain, overweight (100+ lbs), leg swelling, and fatigue
She states: “get me to be able to walk and go shopping and do household chores.”
Lab Review:
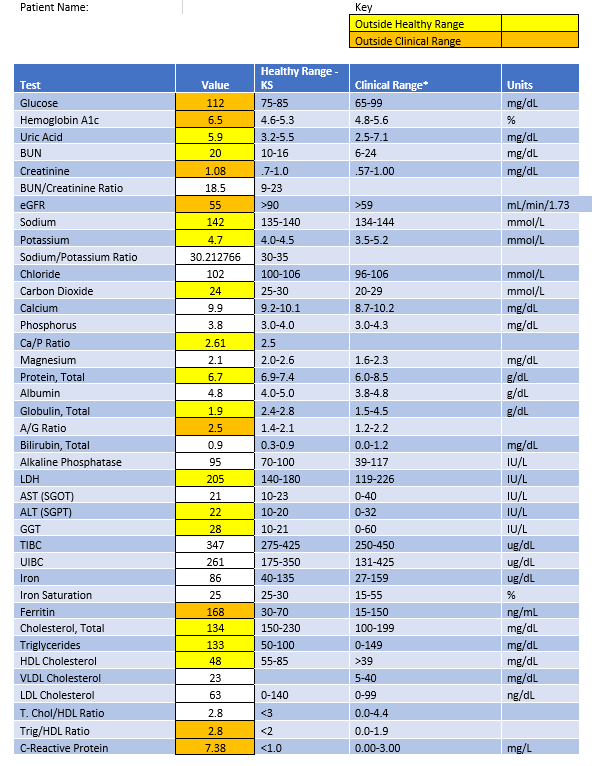
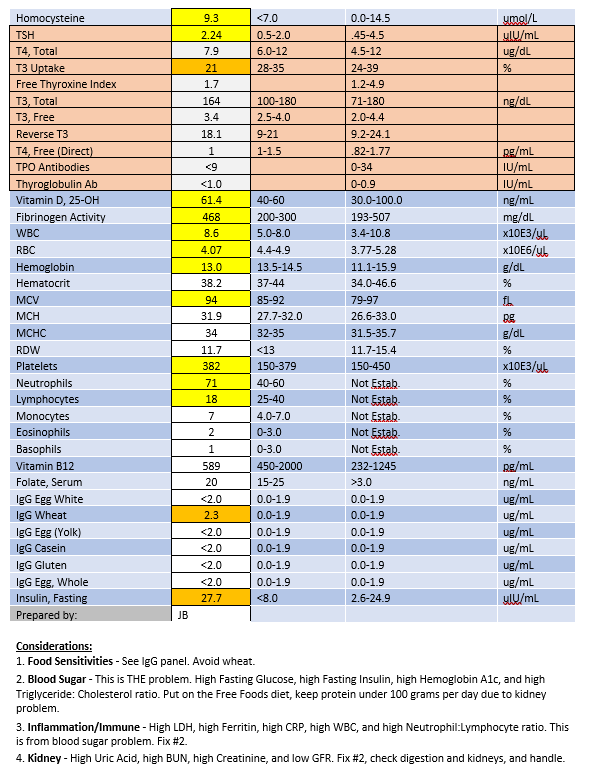
Follow-up: Recheck Chemistry Panel II, Hemoglobin A1c, iron panel, CRP, Thyroid panel, CBC with Differential, and Urinalysis in 4 months.
Nutrition Response Testing Exam
No lock. Start on Free Foods Diet, and check need for supporting supplementation at follow-up visit.
Supplement program at visit 6: AF Betafood – 15, Livaplex – 15
1 Month Follow-up Response to Care
Compliance: She is taking her supplements and following diet very well.
Symptoms: Back pain improved from 8 to 6/10. Ankle swelling is the same. Weight is down 10 lbs, but weight loss has stopped. New symptom: Sinus drainage.
Labs: Kidney markers are worse (eGFR is 43, Creatinine up to 1.31), lipid profile is worse (total cholesterol is lower (128), HDLs down to 41, triglycerides unchanged). Bilirubin is up to 1.4, ALT up to 26.
Her MD Comments: “Her kidney function is being impacted by her diuretic regimen that is trying to manage her edema. She needs to avoid salt.”
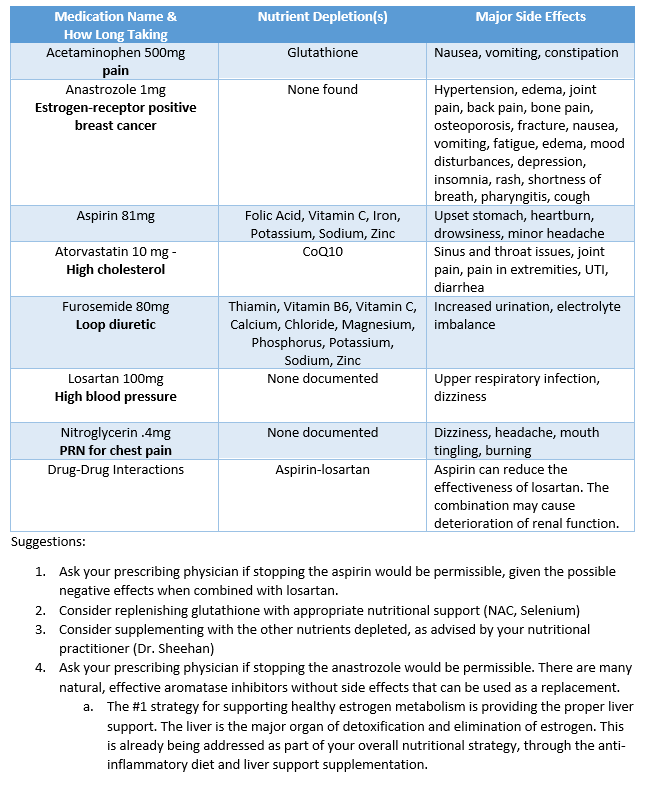
Let’s take a closer look at her meds:
Questions for Comprehension and Practice:
- What is this patient’s nutritional priority issue and why?
- Patient’s MCV is 94, elevated above the optimal range. What is the MCV and how do you explain this elevation nutritionally?
- What could account for this patient’s change in Bilirubin and ALT?
- Which single change in her meds could potentially have the biggest positive impact on her kidney health?